Innovation
Centre for Sustainable Healthcare (CSH) - Taking collective action to deliver low carbon, equitable maternity care
The Challenge
Maternity services account for a significant portion of the NHS’s carbon footprint. With over 673,000 births in 2022, the impact of NHS services on the environment is substantial. Pregnant women and infants are particularly vulnerable to climate change, which exacerbates health complications. Furthermore, significant health inequalities persist, disproportionately affecting women from ethnic minorities and disadvantaged backgrounds. Addressing both the environmental impact and healthcare inequalities is crucial to improving outcomes and creating a more sustainable, equitable healthcare system.
Innovation
As part of CSH’s larger project ‘Taking collective action to deliver low carbon, equitable maternity care’, The Green Maternity Challenge was delivered by CSH in partnership The Royal College of Obstetricians and Gynaecologists (RCOG), The Royal College of Midwives (RCM) and The Sustainable Healthcare Coalition (SHC).
Nine clinical teams in the UK were selected to receive training and mentoring from CSH to develop, plan, run, and measure the impact of a sustainable quality improvement (SusQI) project.
A Green Maternity Showcase was held, and a Green Maternity Conference in March 2025 to share learnings and inspire positive change.
Impact
In the Green Maternity Challenge, CSH helped nine clinical teams in NHS trusts across the UK make a positive impact on sustainable and equitable maternity care.
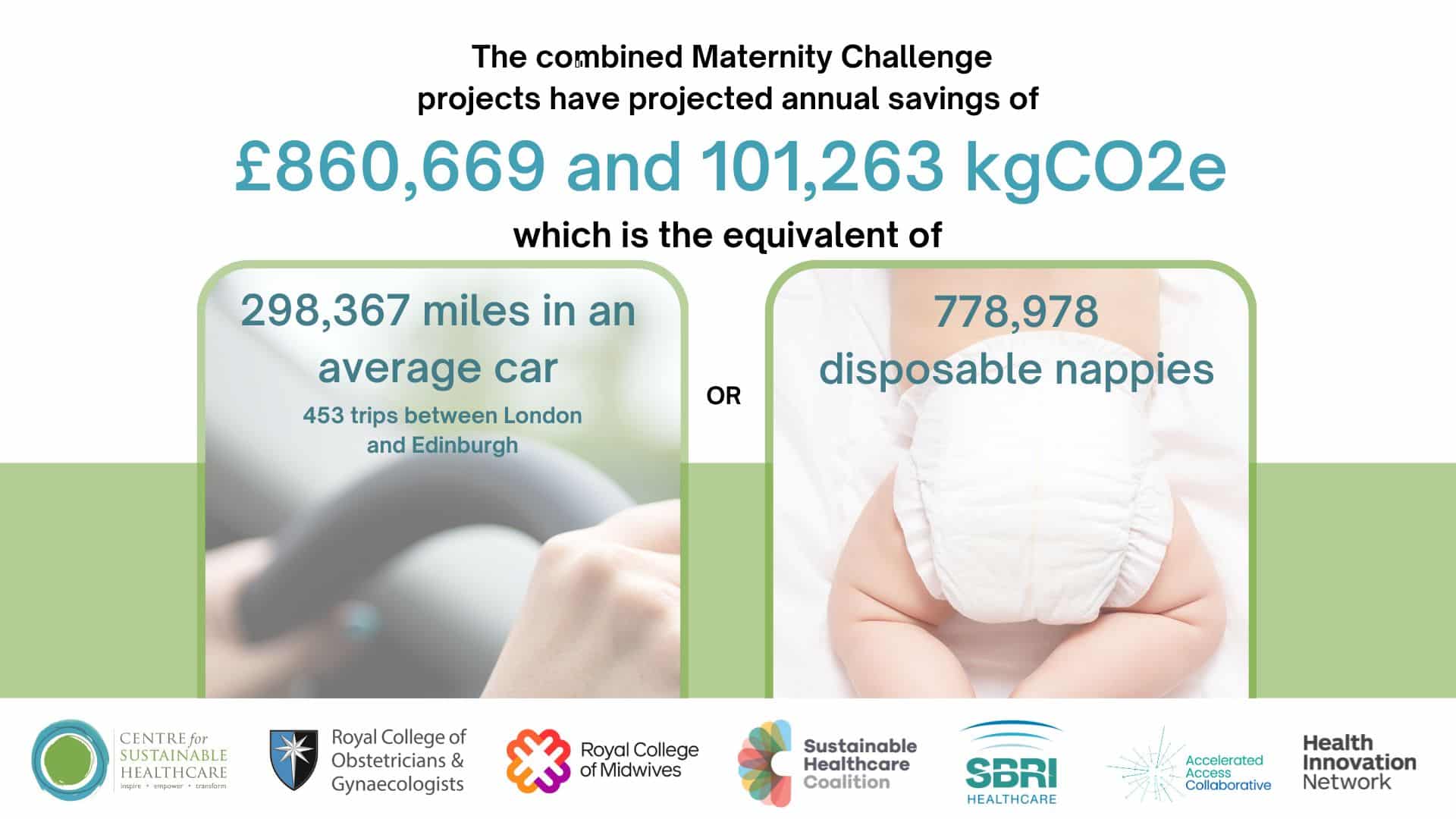
The impact of the Green Maternity Challenge has been significant, with projected annual cost and efficiency savings of £860,669. The projected carbon savings are 101,263 kgCO2e, equivalent to 778,978 disposable nappies. Presentations, videos and reports from the nine projects can be found here.
Example projects include:
-
Norfolk and Norwich University Hospitals NHS Foundation Trust - Reducing the impact of nausea and vomiting in pregnancy - an ambulatory approach
A virtual ward for women with hyperemesis gravidarum, allowing them to receive timely care at home. The carbon footprint of women attending and admitted to the gynaecology ward before the start of the project was 1,804 kgCO2e, compared to 1,266 kgCO2e after the introduction of the virtual ward. By extrapolating this data to a whole year, the greenhouse gas emissions savings are estimated to be 6,461.5 kgCO2e. This data included the number and length of admissions and readmissions, telephone and virtual hub appointments, medications, consumables for treatment and patient travel. The cost of a 24-hour admission to the emergency gynaecology ward is £5,584.03, while the cost of a 24-hour admission to the virtual ward is £117. As above, the projected annual savings are £762,044. -
West Suffolk Hospital - Streamlining the multiple pregnancy pathway
The project focused on optimising antenatal care pathways to reduce unnecessary appointments and investigations, digitising patient information to replace paper-based materials, maximising the use of virtual appointments or appointments being close to home, and improving the consistency and timing of patient information given to increase the provision of high-value and meaningful patient-clinician interaction. The innovation reduced patient travel by offering virtual appointments and consolidating face-to-face visits, resulting in an estimated saving of 150.1 kg CO₂e over the project period. This equates to 28% fewer emissions for patients in this pathway. By using virtual appointments, the project estimated a cost saving per patient of £152.55. It was also found that using a virtual appointment led to a lost productivity saving of £66.93 to the wider UK economy. Extrapolated to the female employment rate of 72.1%, there was a yearly lost productivity saving of £1891.24 regarding wider community. -
Imperial College healthcare NHS trust - Postnatal hypertension made simple and sustainable
The project addressed inconsistencies in prescribing and managing postnatal hypertension, a leading cause of hospital re-admissions by refining clinical guidelines and enhancing staff confidence in the treatment of postnatal hypertension. The intervention reduced the carbon footprint per patient from 205 kgCO₂e to 88 kgCO₂e, saving 117 kgCO₂e per patient. When extrapolated to 500 women, which accounts for 10% of the number of deliveries at Queen Charlotte’s and Chelsea hospital, reflective of the average number of women affected by hypertensive disorders, this means that there could be savings of 58,645 kgCO2e, equivalent to 172,795 miles driven. The project decreased the average cost of a 14-day antihypertensive prescription from £2.79 to £2.46 per patient. Additionally, the average cost of blood tests per patient was reduced from £28.60 to £13, potentially leading to savings of £14,300 if scaled across the population. Additional savings could also be seen from shorter inpatient stays, reduced financial cost for example due to transportation. Post intervention, the average postnatal hospital stay was reduced by 2.6 days. The number of blood tests per patient decreased by an average of 2.92. Notably, the proportion of patients discharged on multiple antihypertensives dropped from 28% to 0%, and unplanned reviews and readmissions were eliminated.
Date published
June 2025

